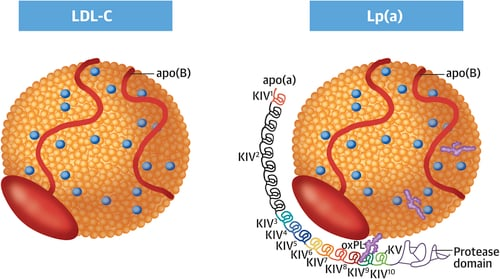
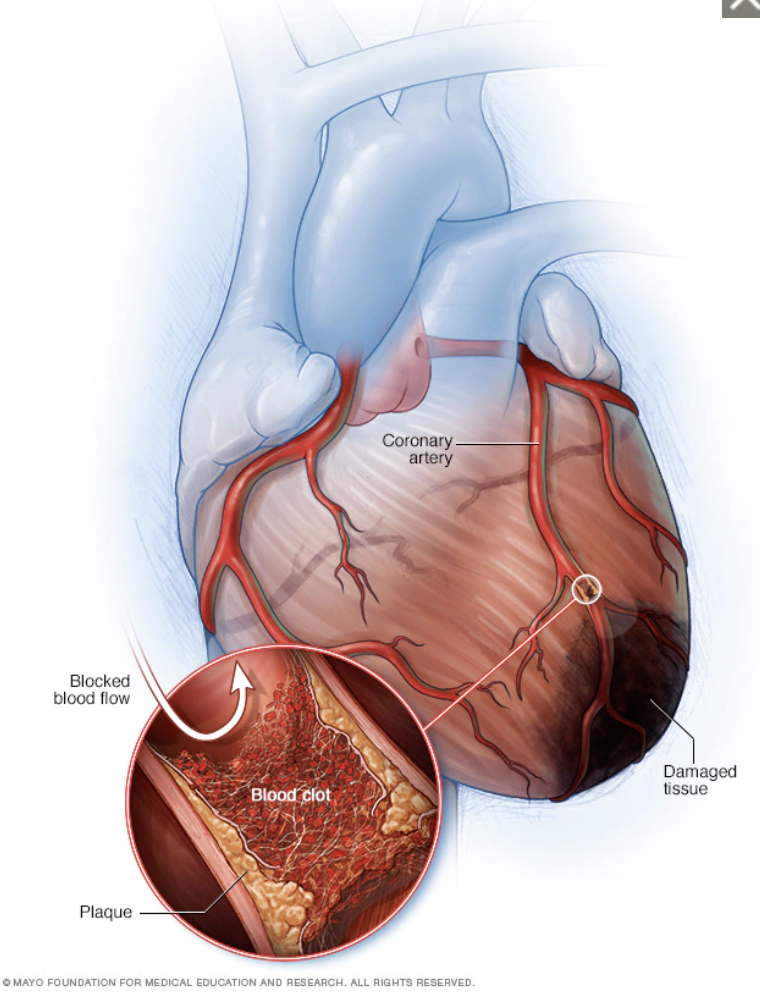
Low Density Lipid (LDL) Cholesterol is the main cause of atherosclerosis, which is the abnormal deposition of cholesterol in the arterial wall. Atherosclerosis is the basis of cardiovascular disease.
What is a normal LDL cholesterol for a human?
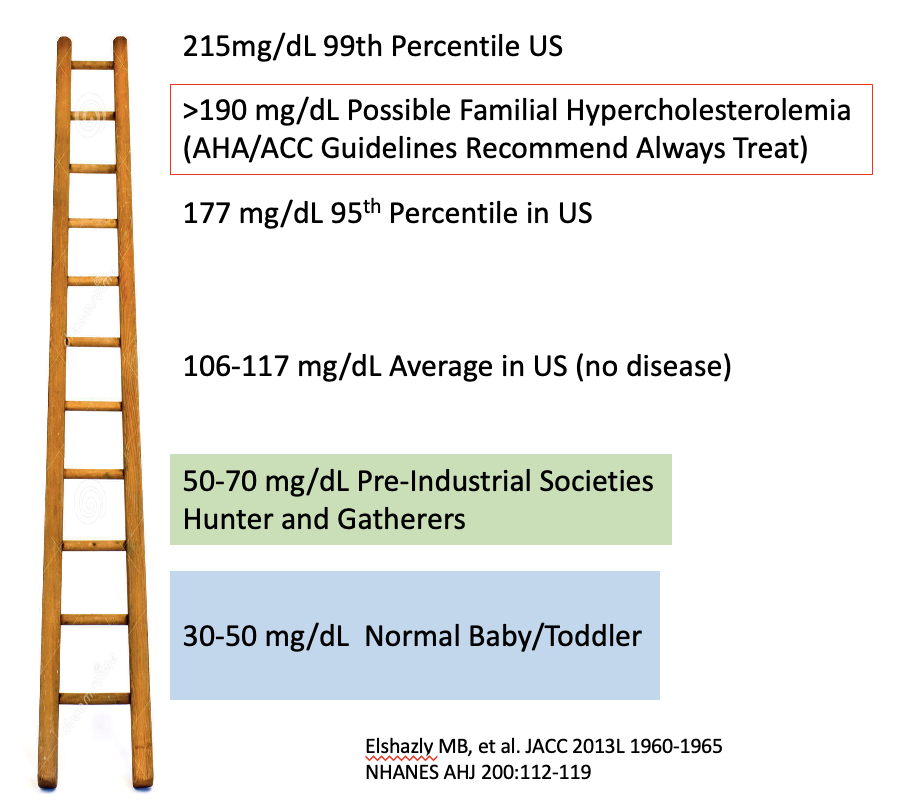
This is a an interesting question and we can look at a few pieces of evidence that support the LDL should be very low (<70 mg/dL). For example, when babies are born, the LDL is between 30-50 mg/dL. This remains true up until ~3 years of age. After the LDL does rise. There are theories that increased dietary sugar intake increase PCKSk9 expression in the liver, which in turns decreases LDL receptors. Less LDL receptors causes less LDL particles to be removed from the blood stream.
Total cholesterol is low in pre-industrial societies such as Hazda and Inuit. These societies still practice a Hunter-Gatherer lifestyle. Although they do eat animal proteins (especially the Inuit), the diet does not contain processed foods. These diets have significantly more fiber intake. People in these societies can lives in their 70-80’s without evidence of atherosclerosis.
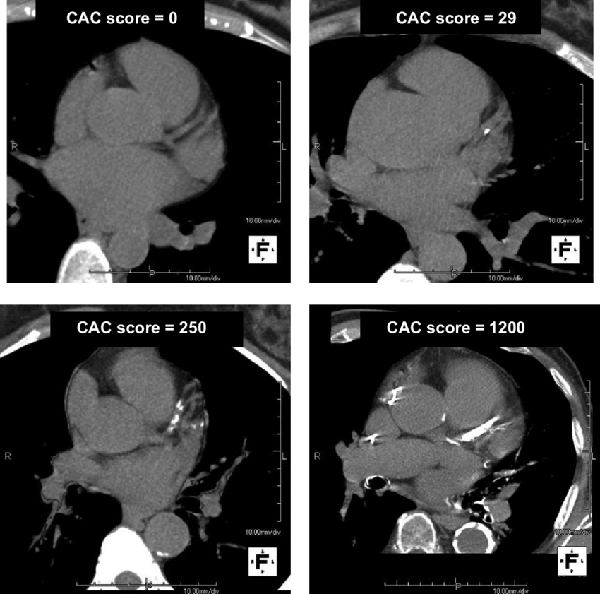
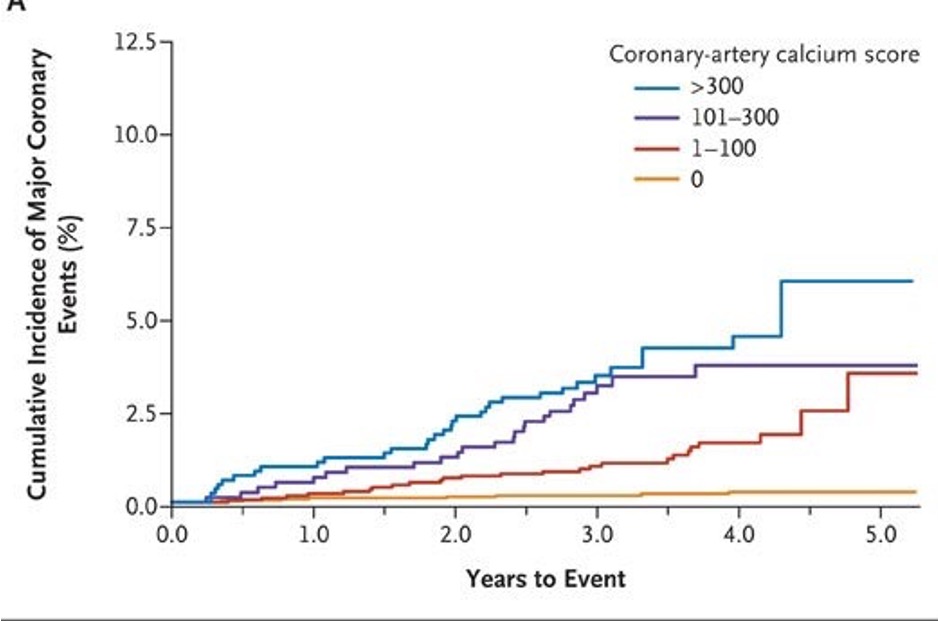
One amazing study of the Tsimane, a Bolivan tribe, found 5x lower rates of coronary artery disease than the US population. These research scanned 705 people with a CT scanner to determine coronary artery calcifications. 85% of the study group had Zero Calcium! Of note, the average LDL of the Tsimane was 91 mg/dl.
And when you compare total cholesterol among humans versus primates and mammals, you see that there is a large difference.

So we can conceptualize LDL levels on a ladder. Higher on the ladder, higher the risk of cardiovascular disease. The average LDL cholesterol in the US population on 106-117 mg/dL which is about 40-60% higher than a hunter gatherer society.
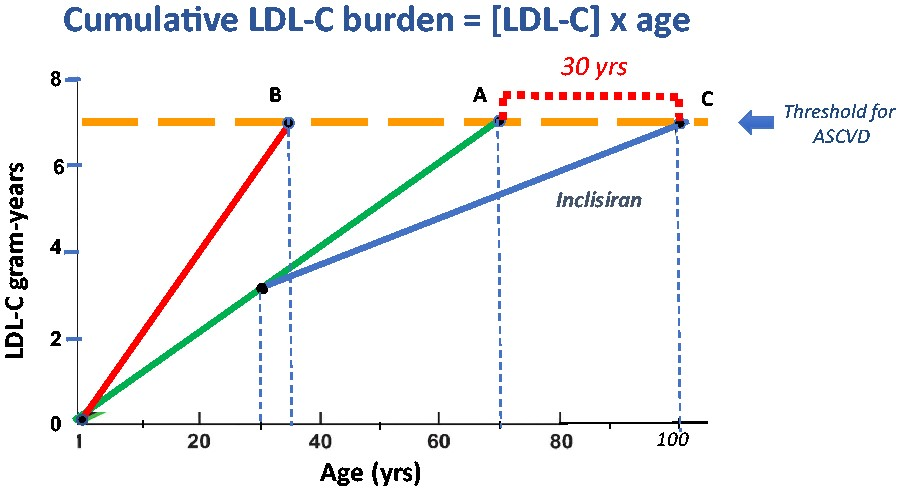
Therefore to consistently prevent atherosclerosis, maintaining a low LDL cholesterol is a key strategy. This is why Dr. Baunwald has suggested using yearly shots of incliseran to prevent cardiovascular disease. Similar to categorizing the severity of a smoker’s history in pack-years, Dr. Braunwald suggests we view cholesterol-years as an expression of cholesterol burden. The yellow line represents the cumulative exposure of a LDL 7 gm for 70 years. If we can reduce the LDL cholesterol early in life, we can delay the onset of atherosclerotic disease for 30 years.
I don’t think society or the healthcare system is ready to give every adult a yearly shot of incliseran. But we can all take steps to improve our diet to lower the LDL as much as possible. I suggest a Mediterranean style diet which is low in process foods and high in fiber.